Exposure to allergens in the research environment, particularly in animal facilities, poses serious health risks to the workforce. Laboratory animal allergy (LAA) stands out as a paramount occupational concern, affecting up to one-third of personnel working with laboratory animals. This article delves into the intricacies of LAA, shedding light on the science, implications, and strategies for effective allergen management in line with established industrial hygiene principles.
The Gravity of Laboratory Animal Allergens
LAA, recognized as a consequential occupational disease, impacts a considerable number of individuals exposed to lab animals. The allergens are not just confined to the animals themselves. Materials like animal bedding, which come into contact with laboratory animals, can become a hotbed for allergens. From dander, hair, saliva, and urine – various allergen sources from these animals can be the triggers. For instance, rodent urinary allergens, if inhaled or in direct contact with the skin, pose significant health hazards.
The crux of exposure risk stems from three core parameters: intensity (or concentration), duration, and exposure routes, often linked directly to specific job tasks and responsibilities. Inhalation of airborne allergens, or aeroallergens, is the predominant way workers get exposed. The size of these aeroallergen particles plays a pivotal role in how they impact the respiratory system, with varying sizes depositing in different regions of the respiratory tract.
Toward Comprehensive Exposure Control
Addressing LAA involves a multi-faceted approach, closely mirroring strategies for managing traditional occupational hazards. These include:
- Engineering Controls: Facility design, proper ventilation, and other structural measures.
- Administrative Controls: Addressing the human factor with appropriate work practices, training, and operational guidelines.
- Personal Protective Equipment (PPE): Offering an immediate line of defense for workers.
Notably, it’s not just about curbing direct exposure. Indirect or “fugitive” exposures from occupational sources, impacting individuals not directly involved in animal care, should be on the radar as well.
Why Addressing Laboratory Animal Allergens Matters
Considering the potent nature of laboratory animal allergens, where even nanogram concentrations can trigger symptoms among sensitive individuals, implementing a robust control strategy is critically important. A combination of understanding the sources, recognizing exposure routes, and integrating tailored control measures can pave the way for safer work environments, ultimately minimizing the prevalence of LAA.
To those in the research community, especially those working closely with laboratory animals, understanding the risks and arming oneself with the best practices is more than just professional diligence – it’s a commitment to the well-being of oneself and the larger community.
Understanding Laboratory Animal Allergens
Laboratory animal allergens are a topic of great concern, especially for those engaged in research environments. The negative health implications are profound, and it’s imperative for individuals working around animals to be informed.
What Exactly Are Animal Allergens?
Animal allergens refer to proteins present in a variety of animal-based substances such as:
- Urine
- Fur
- Saliva
- Feathers
- Blood
- Feces
- Dander (minute scales from hair, feathers, or skin)
Exposure to these allergens can trigger an exaggerated immune response in individuals predisposed to allergies. These allergies can sometimes take considerable time — from weeks to years — to manifest. Extreme cases might even evolve into conditions like asthma, with some employees having to significantly adjust their lives due to severe symptoms. Lab animals like rats, cats, rabbits, dogs, ferrets, guinea pigs, and hamsters produce particularly potent allergens.
Exposure to Animal Allergens
The risk of exposure to allergens isn’t limited to direct interaction with animals. Inhalation of allergens is an especially powerful form of exposure, often released into the atmosphere when dander or fur sheds or when materials containing these allergens are disturbed. Activities like changing cages, dumping cages, or conducting animal procedures can release these allergens into the air. Thus, even those who aren’t directly handling animals, but are in the vicinity, might be exposed.
Who Is Most At Risk?
All individuals working directly or indirectly with laboratory animals are at an elevated risk of developing allergies. However, some groups face a heightened threat:
- Those with a history of allergies or hay fever.
- Individuals allergic to domestic animals, like cats and dogs.
- Professionals with a past of working with animals, such as lab animal workers or livestock handlers.
- People exposed to tobacco smoke.
Between 11 to 44 percent of animal workers may develop allergic reactions. Of these, a significant number might eventually develop asthma, which sometimes persists even after ending exposure.
Identifying Symptoms
A wide range of symptoms might manifest, either alone or in combination:
- Respiratory symptoms like nose, eye, and throat irritation, sneezing, coughing, chest tightness, and shortness of breath.
- Skin-related symptoms include itchy rashes and hives. An extreme form of sensitization is anaphylactic shock, characterized by sudden breathing or swallowing difficulties.
Reducing Exposure: Best Practices
Prevention is key. Awareness of allergens’ sources and understanding individual risks is the first step. Before working in animal-related environments, complete the Animal Use Medical Screening.
Engineering controls – Tools like biological safety cabinets, cages with filter tops, and individually ventilated cage systems (IVCs)- are instrumental in capturing allergens. On the other hand, work practice controls involve adopting measures like thorough hand washing after handling animals, wet-wiping work surfaces, wearing PPE, and more.
Addressing Symptoms
It’s crucial to consult the employee health center immediately if you notice any symptoms. Symptoms can appear or intensify over prolonged periods, even up to a decade. As the exposure continues, symptoms might worsen. Hence, it’s essential to regularly consult with healthcare providers about potential risks and inform them about your proximity to animals in your professional setting.
Isolation and Enclosure
Isolation and enclosure involve physically separating the allergen source from the worker. For instance, animal cages or housing systems can be designed to be completely sealed or contained, ensuring that allergens do not escape into the work environment. This method can be highly effective in reducing the exposure of workers to allergens. Many facilities use IVCs to ensure a controlled air environment, thereby preventing the spread of allergens.
Ventilation
Effective ventilation systems are pivotal in controlling and reducing workers’ exposure to aeroallergens. Local exhaust ventilation, such as canopy hoods over cage dumping areas, can capture airborne contaminants at the source and expel them from the workplace. Dilution or general ventilation, which involves replacing contaminated air with fresh air, can also be effective, especially when combined with local exhaust systems.
Ventilation systems should be designed around the facility’s specific needs, with regular maintenance and monitoring to ensure they operate efficiently. Properly placed high-efficiency particulate air (HEPA) filters can trap allergenic particles, preventing them from being recirculated in the environment.
Administrative Controls and Work Practices
Apart from engineering controls, certain administrative actions and work practices can be implemented to reduce allergen exposure:
- Rotation of Duties: Rotate employees through jobs that have high allergen exposure to minimize the duration of their exposure.
- Training and Education: Regularly train and educate employees on the risks of allergen exposure, proper handling of animals, and the correct use and maintenance of protective equipment.
- Housekeeping: Regular cleaning of the facility using wet methods or vacuum cleaners equipped with HEPA filters can reduce settled allergens that may become airborne.
- Hygiene: Providing facilities for workers to shower and change clothes before leaving work can prevent allergens from being carried home.
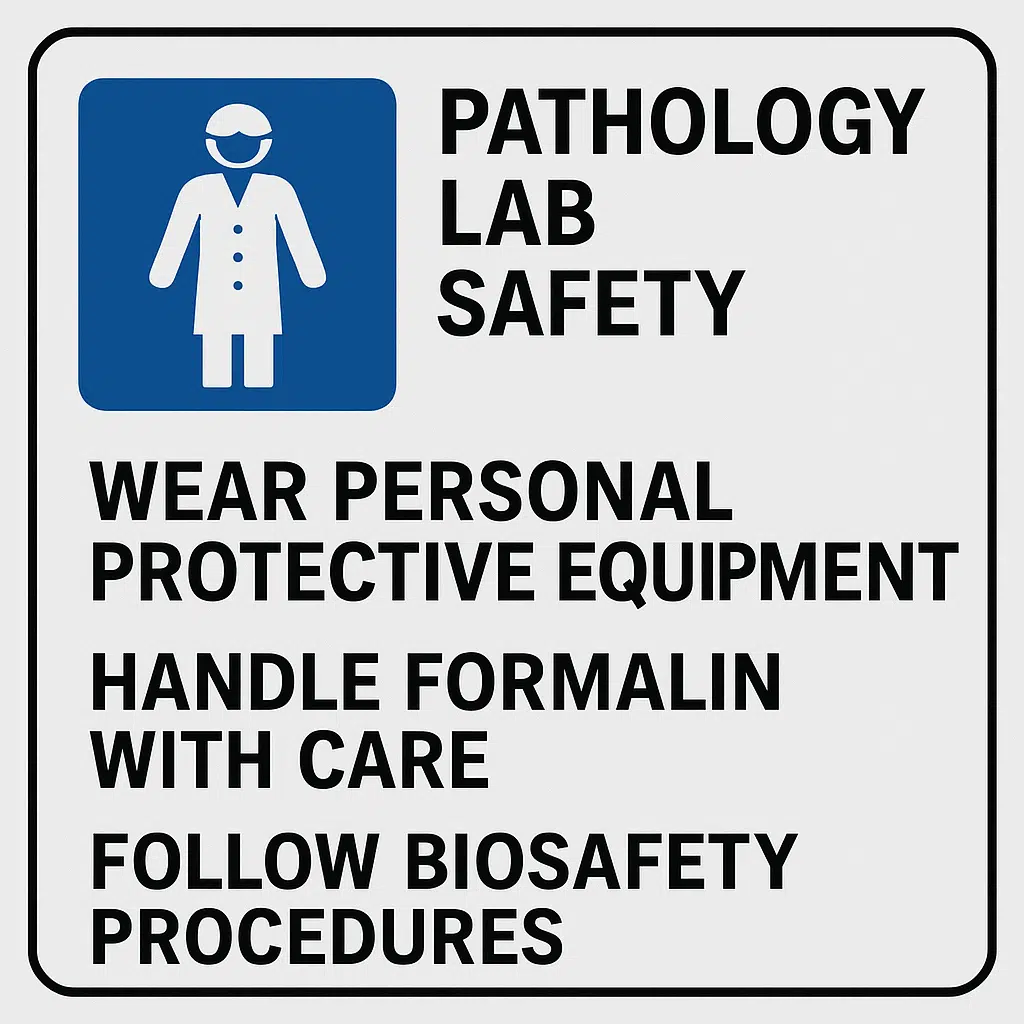
Personal Protective Equipment
Where engineering and administrative controls are not feasible or do not offer complete protection, PPE can serve as an additional protective barrier. Respirators, gloves, lab coats, and eye protection can be effective if chosen correctly and used consistently. However, PPE is considered the last line of defense and should not be the primary means of protection.
It is imperative to select the appropriate type of PPE based on the nature of the job and the level of allergen exposure. Furthermore, regular training and fit-testing, especially for respirators, are vital to ensuring effectiveness.
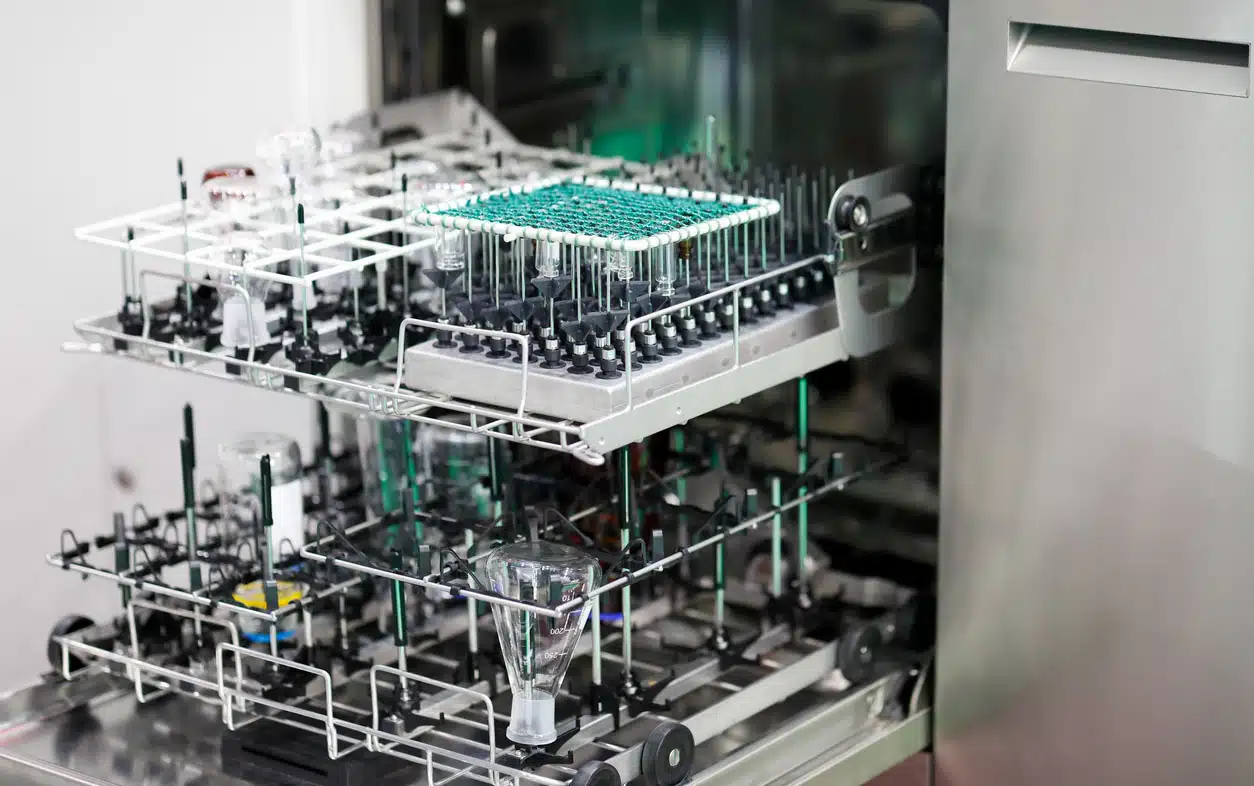
Streamlining Bedding Disposal: A Blend of Safety and Efficiency
Animal research facilities have long grappled with the challenge of bedding disposal. At the heart of this is the critical balance between ensuring the safety of technicians and maintaining efficiency. The vast landscape of bedding disposal systems reveals many good intentions that sometimes miss the mark. So, what is the ideal bedding disposal system? Let’s take a closer look.
Protecting Technicians from Respirable Dust
While many products and systems are available in the market, not all are designed with the end user in mind. Protecting staff from respirable dust is a non-negotiable aspect of animal facilities. Traditional methods, such as the simple barrel or dump cart, although easy for technicians, inadvertently release significant amounts of allergens, dander, and dust. The risk associated with these methods is immense, especially when you consider the potential for fecal waste, bedding, and paper particle aerosolization. Yet these methods persist in many facilities.
The Ideal Disposal System
The perfect bedding disposal system would seamlessly integrate the vacuum system’s efficiency, the biological safety cabinet’s security, and the 55-gallon barrel’s simplicity. But it’s all about striking the right compromise. This compromise should not lead to systems gathering dust in storage areas because they overcomplicate the technician’s workday.
Two systems have emerged as leaders in this space. The first are vacuum-based systems that transport waste to remote storage units. The second are dump stations that combine a biological safety cabinet’s features with a simple hood where animal bedding is deposited — while also isolating the worker from dust created by the bedding. These stations allow waste to be safely deposited into a centrally located barrel or box before easy disposal.
The Mobile Bedding Disposal System: Bridging the Gap
Modern animal research facilities constantly pursue equipment that can enhance their operational efficiency while ensuring safety for both the animals and the technicians. The mobile bedding disposal system is a powerful piece of equipment in this respect.
Such stations have carved a niche by seamlessly merging aspects like safety, adaptability to varying sizes, cost-efficiency, and robustness. Technicians applaud them for their efficient operation, and facility managers highly regard their adherence to health and safety regulations.
Highlighting the attributes of these disposal stations:
- Active Airflow Technology: This feature safeguards operators during the removal of waste bins. It directs airflow away, minimizing the risk of allergen exposure.
- Universal Cage Compatibility: A hallmark of design excellence, these stations can fit rodent cages of varying size, ensuring effective disposal without allergen release.
- Multi-Stage Filtration: These disposal systems integrate a multi-stage filtration mechanism that culminates with an H14 HEPA filter, ensuring thorough allergen capture.
- Optimized Workflow and Cleanability: The layout promises a generous workspace, uncomplicated cage breakdown, and straightforward cleaning. Additionally, its user-centric design makes installations a breeze even for those not technically inclined.
- Mobility: Many animal bedding disposal stations can be moved easily to streamline workflows.
ARES – Pioneering Excellence in Animal Bedding Disposal
In the rapidly evolving landscape of animal research, ARES has consistently emerged as a beacon of industry leadership and unparalleled expertise in animal bedding disposal. This distinction is not accidental. ARES’s association with reputable brands such as Sychem and Park Bio proves its commitment to quality and innovation. Units provided by these brands have undergone rigorous field testing, ensuring they can handle real-world challenges effectively. Such resilience and performance are exactly why they enjoy widespread endorsement from animal researchers worldwide.
However, what sets ARES apart is its bespoke approach to client needs. ARES understands that each facility is unique, with its own set of challenges and constraints. Whether it’s the spatial layout, specific safety requirements, or budget considerations, ARES dives deep to understand the specifics. With this granular understanding, they provide solutions that are not just effective but also tailor-made for each facility.
Protecting the health and well-being of workers in animal research environments is a responsibility that ARES does not take lightly. In partnership with facility managers, ARES ensures the implementation of the best bedding disposal options that offer maximum protection without compromising efficiency.
So, when you think of equipping your facility with the best in animal bedding disposal, think ARES. Its rich industry experience, collaboration with leading brands, and dedication to customer-specific solutions ensure that your facility’s needs are met with precision, care, and within budget.